GD-52: Design Guide for Nuclear Substance Laboratories and Nuclear Medicine Rooms
Preface
This guidance document provides information for a recommended approach for meeting the requirements related to site description and room design under paragraphs 3(1)(d) and 3(1)(l) of the Nuclear Substances and Radiation Devices Regulations and performing shielding design analyses as a component of keeping doses As Low As Reasonably Achievable (ALARA) pursuant to paragraph 4(a) of the Radiation Protection Regulations.
This guidance document provides design recommendations for a nuclear medicine room or a nuclear substance laboratory where unsealed nuclear substances are to be used, and an approach for submitting the proposed design to the Canadian Nuclear Safety Commission (CNSC).
It includes guidance on finishing and fixtures, plumbing, storage, security, ventilation, shielding, and dose estimation for basic, intermediate, high, and containment level nuclear substance laboratories and nuclear medicine rooms.
Key principles and elements used in developing this guide are consistent with national and international standards. The complete list is included in Associated Documents; examples include Laboratory Biosafety Manual from the World Health Organization (WHO); and CSA Z316.5-04—Fume Hoods and Associated Exhaust Systems from the Canadian Standards Association (CSA).
Nothing contained in this document is to be construed as relieving any licensee from pertinent requirements. It is the licensee’s responsibility to identify and comply with all applicable regulations and licence conditions.
Contents
- 1.0 Introduction
- 2.0 Licensing Process for Nuclear Substance Laboratories and Nuclear Medicine Rooms
-
3.0 Using the Design Assessment Form (DAF)
- 3.1 Supplementary Information for Part A of the Design Assessment Form
- 3.2 Supplementary Information for Part F of the Design Assessment Form
- Appendix A: Dose Conversion Factors (DCF) and Annual Limits on Intake (ALI) for Common Nuclear Substances
- Appendix B: Calculating Dose Estimates
- Appendix C: Design Assessment Form
- Glossary
- References
- Additional Information
1.0 Introduction
1.1 Purpose
This guidance document provides information for a recommended approach for meeting the requirements related to site description and room design under paragraphs 3(1)(d) and 3(1)(l) of the Nuclear Substances and Radiation Devices Regulations and performing shielding design analyses as a component of keeping doses As Low As Reasonably Achievable (ALARA) pursuant to paragraph 4(a) of the Radiation Protection Regulations.
1.2 Scope
This guidance document provides design recommendations for a nuclear medicine room or a nuclear substance laboratory where unsealed nuclear substances are to be used, and an approach for submitting the proposed design to the Canadian Nuclear Safety Commission (CNSC).
It includes guidance on finishing and fixtures, plumbing, storage, security, ventilation, shielding, and dose estimation for basic, intermediate, high, and containment level nuclear substance laboratories and nuclear medicine rooms.
1.3 Relevant Regulations
The provisions of the Nuclear Safety and Control Act (NSCA) and the regulations made under the NSCA relevant to this guide are as follows:
- Subsection 24(4) of the NSCA states that “No licence may be issued, renewed, amended or replaced unless, in the opinion of the Commission, the applicant (a) is qualified to carry on the activity that the licence will authorize the licensee to carry on; and (b) will, in carrying on that activity, make adequate provision for the protection of the environment, the health and safety of persons and the maintenance of national security and measures required to implement international obligations to which Canada has agreed.”
- Section 3 of the General Nuclear Safety and Control Regulations provides a list of information which an application for a licence shall contain.
- Paragraph 12(1)(c) of the General Nuclear Safety and Control Regulations states that “Every licensee shall take all reasonable precautions to protect the environment and the health and safety of persons and to maintain security.”
- Paragraph 3(1)(d) of the Nuclear Substances and Radiation Devices Regulations states that “An application for a licence in respect of a nuclear substance or a radiation device, other than a licence to service a radiation device, shall contain… (d) the proposed location of the activity to be licensed, including a description of the site.”
- Paragraph 3(1)(l) of the Nuclear Substances and Radiation Devices Regulations states that “An application for a licence in respect of a nuclear substance or a radiation device, other than a licence to service a radiation device, shall contain, where the application is in respect of a nuclear substance that is an unsealed source and that is to be used in a room, the proposed design of the room.”
- Subparagraph 4(a)(iii) of the Radiation Protection Regulations states that “Every licensee shall implement a radiation protection program and shall, as part of that program, (a) keep the amount of exposure to radon progeny and the effective dose and equivalent dose received by and committed to persons as low as is reasonably achievable, social and economic factors being taken into account, through the implementation of… (iii) control of occupational and public exposure to radiation”.
2.0 Licensing Process for Nuclear Substance Laboratories and Nuclear Medicine Rooms
As part of the process to obtain a licence for the use of an unsealed nuclear substance, applicants must submit a completed licence application in accordance with section 3 of the General Nuclear Safety and Control Regulations, section 3 of the Nuclear Substances and Radiation Devices Regulations, and section 4 of the Radiation Protection Regulations. As part of the licence application, applicants must submit the proposed design of the room in which unsealed nuclear substances will be used.The Design Assessment Form (DAF) provided in Appendix C of this document assists licence applicants with the submission of the proposed design of their nuclear medicine room or nuclear substance laboratory. A DAF should be completed for any new construction or major renovation (such as demolishing walls, changes to existing shielding, or installing new fumehoods; for additional information, contact a CNSC Licensing Specialist) and enclosed with the new application or a request for amendment. A good laboratory design facilitates adherence to safe policies and procedures.
The completed DAF should be submitted to the CNSC as early as possible in the design stage in order to facilitate the processing of the licence application or amendment. If multiple rooms are to be constructed or renovated and are to be of similar design and function, only one DAF needs to be submitted. Where more than one laboratory or room for the handling of unsealed sources is to be constructed or renovated, and the designation or use of each is different, a separate DAF should be submitted for each laboratory or room. CNSC staff may request additional information after the initial design or renovation assessment is complete.
3.0 Using the Design Assessment Form (DAF)
The DAF is divided into the following categories:
- A
- General Information;
- B
- Finishing and Fixtures;
- C
- Plumbing;
- D
- Security;
- E
- Ventilation;
- F
- Shielding/Dose Control; and
- G
- Miscellaneous.
The guidelines set out in the DAF are considered to be good design features that contribute to the optimization of radiation protection and keeping doses ALARA. The plans for the design, construction, or renovation of all nuclear substance laboratories and nuclear medicine rooms should incorporate the guidelines applicable to the work to be performed.
Any proposed variation from the guidelines should be supported by additional information to demonstrate, to the satisfaction of CNSC staff, that the guideline is not applicable due to the nature of the proposed activities, or that the guideline is addressed by alternative measures that provide an equivalent degree of safety.
3.1 Supplementary Information for Part A of the Design Assessment Form
3.1.1 Classification of Rooms
Part A of the DAF asks for general information, including the classification of the room in which the nuclear substance will be used. Rooms where unsealed nuclear substances are used in industrial, medical, or academic research settings are classified by the CNSC as basic, intermediate, high, or containment-level laboratories, or as nuclear medicine rooms, depending on the amount of nuclear substances handled in the room and on the nature of the work performed.
All areas, rooms, and enclosures where more than one exemption quantity1 of an unsealed nuclear substance is used at a single time are classified by the CNSC according to Table A. If the area, room, or enclosure is used only for storage of unsealed nuclear substances or for the use or storage of sealed nuclear substances or radiation devices, the classifications in Table A do not apply.
As per licence conditions, nuclear medicine departments and clinics shall designate all rooms that will be used to prepare nuclear substances for administration to a person, or to administer the nuclear substance to a person, as “nuclear medicine” rooms.
With respect to veterinary nuclear medicine departments or clinics, CNSC classifies the area or enclosure as Basic, Intermediate, High, or Containment, according to Table A:
- Any area or enclosure where animals treated with more than one exemption quantity of a nuclear substance are housed, and
- Any area or enclosure where more than one exemption quantity of an unsealed nuclear substance is used at a single time.
| Room Classification | Description |
|---|---|
| Basic Level Laboratory | The quantity of unsealed nuclear substance used at a single time does not exceed 5 times its corresponding annual limit on intake (ALI). |
| Intermediate Level Laboratory | The quantity of unsealed nuclear substance used at a single time does not exceed 50 times its corresponding ALI. |
| High Level Laboratory | The quantity of unsealed nuclear substance used at a single time does not exceed 500 times its corresponding ALI. |
| Containment Level Laboratory | The quantity of unsealed nuclear substance used at a single time exceeds 500 times its corresponding ALI. |
| Nuclear Medicine2 | The nuclear substance is prepared for or administered to a person. |
Note that the appropriate ALI value is the one that best represents the risks associated with the nuclear substance. If it cannot be determined whether the greater risk is related to inhalation or ingestion of the substance, then the most restrictive value should be used. For a list of Annual Limits on Intake (ALIs), refer to Appendix A.
For licence applications, all pertinent information must be submitted. The DAF is provided to facilitate the process of submitting the pertinent information. Once the licence has been issued, future basic-level laboratories do not require submission of the information in the DAF. For all other room classifications, future additional rooms or renovations require submission of all pertinent information and it is recommended that a completed DAF be included.
1 For a definition of exemption quantities, refer to section 1 of the Nuclear Substances and Radiation Devices Regulations. For a list of exemption quantities, refer to Schedule 1, column 3 of those regulations.
2 In the context of this guide, the term “nuclear medicine room” refers strictly to any area or enclosure that is used for the preparation of, or medical administration of, nuclear substances to persons via injection, inhalation, or ingestion, for the purpose of diagnosing or treating disease and for human research studies (excluding medical diagnostic x-rays or the medical use of sealed nuclear substances for brachytherapy or teletherapy treatments).
3.2 Supplementary Information for Part F of the Design Assessment Form
As per subparagraph 4(a)(iii) of the Radiation Protection Regulations, the concept of optimization of radiation protection (i.e., ALARA) must be considered when designing any facility where nuclear substances will be used. With nuclear medicine, this is especially important given that the source, once administered in a person, will not be in a fixed location. At the planning and design stage, the impact of design decisions on potential doses to persons (excluding the patient) should be a prime consideration.
Assessments of applications with respect to any nuclear medicine room, any high or containment level laboratory, or any area or enclosure associated with veterinary nuclear medicine will include the review of dose estimates for persons (excluding the patient) in the areas where the unsealed nuclear substances will be used. The purpose of this section is to provide guidance on how to determine and demonstrate that radiation dose estimates are ALARA prior to carrying out any licensed activities.
CNSC document G-129 rev 1, Keeping Radiation Exposures and Doses “As Low As Reasonably Achievable (ALARA)”, provides guidance on keeping doses ALARA.
3.2.1 Dose Estimates for Nuclear Medicine Room Design Applications
Dose estimates will only give a reasonable representation of potential exposures if the parameters are examined carefully to ensure they properly characterize the design and operation of the facility. The applicant or licensee should consider the following parameters when calculating the dose estimates resulting from its intended operations:
- Layout and construction;
- Locations at which these nuclear substances and activities will be used;
- Distances between the nuclear substance or patient and the occupied locations of other persons;
- Occupancy of the other rooms in the nuclear medicine department and surrounding areas by persons other than the patient (if the facility has more than one floor, consider occupancy above and below);
- Nuclear substances and activities (Bq) to be used for the nuclear medicine procedures performed; and
- Maximum number of patients per procedure to be treated, annually.
3.2.1.1 Dose Estimates for Conventional Diagnostic Nuclear Medicine—A Five-Step Method
The following 5-step method for calculating dose estimates is a suggested approach only; it does not restrict the applicant from using other approaches. Each of these five steps is described in greater detail in Appendix B using an example to illustrate the overall method.Step 1) Obtain architectural drawings or make an accurate, scaled and dimensioned drawing of the facility and surrounding areas.
The drawings need to show the locations where significant quantities of nuclear substance will be present, and those occupied locations where persons other than the patient might be expected to be exposed to radiation as a result of the nuclear medicine procedures.
Step 2) Identify the key locations where nuclear substances are to be used and the number of procedures, as well as the typical activity per procedure, for each of these locations.
The key locations include both the rooms where any nuclear substance will be administered to the patient and the main post-administration locations occupied by patients, such as injection rooms, designated waiting areas, gamma camera rooms, and treadmill rooms. For each location and type of procedure performed:
- Determine the nuclear substance and typical activity (MBq) to be used for each procedure; and
- Estimate the approximate number of procedures to be performed per year.
Step 3) Identify the purpose, type of occupancy and occupancy factor of those areas within, or in the immediate vicinity of, the nuclear medicine department, that will be occupied while nuclear substances are in use.
For each area in which persons (other than the patient) would be expected to receive a radiation dose as a consequence of nuclear medicine activities, determine:
- What the area is used for (e.g., reception desk, waiting room, gamma camera room, washroom, etc.);
-
The persons who are normally present in the area, including:
- Staff who are nuclear energy workers (NEWs), such as nuclear medicine technologists;
- Staff who are non-NEWs and are occupationally exposed; and
- Non-NEWs who are members of the general public and are non-occupationally exposed, such as persons accompanying patients.
- The occupancy factor (T) for each location and exposed group (i.e., the fraction of total time during which a radiation field may be present at a particular location, for which another individual may be present at that location). For additional information, refer to the National Council on Radiation Protection and Measurements (NCRP) Report No. 151: Structural Shielding Design and Evaluation for Megavoltage X- and Gamma-Ray Radiotherapy Facilities.
When evaluating T, an important consideration is whether or not a person may be at the location of interest while there is a radiation field present in that area.
Step 4) Estimate the radiation dose rates produced in each potentially occupied area.
Two basic methods are used to estimate the radiation dose rates to which a person (excluding the patient) will be exposed as a result of typical nuclear medicine operations.
The first method is to take direct measurements of the dose rates in surrounding areas, using a sufficiently sensitive, properly calibrated radiation survey meter or other, equivalent method. The type, model, energy range, and energy response of the dose rate meter to be used should be provided. This method is generally useful when evaluating an existing department, or when making a comparative analysis for designing a new room or department that is very similar in layout and design to an existing site. It is particularly useful when an applicant needs to analyze the impact of proposed changes, such as increased workload or changes to the facility layout.
The second method is a mathematical approach that relies, for example, on the known physical properties of the nuclear substances being used, the distances to each occupied area and the shielding properties and thickness of the building materials. This method is generally useful when designing a new room or department. This technique is described in detail in the example provided as Appendix B of this guide.
Step 5) Extrapolate the measured or calculated dose rates at each location to annual doses for the persons who may occupy each area, based on the projected facility workload and the occupancy factor.
Patients typically occupy several different locations over the course of the nuclear medicine procedure and may contribute to the dose received by a person occupying a single location (e.g., the dose from patients in the injection room, scanner rooms, and post-injection waiting areas may all contribute to the dose received by the receptionist at the front desk). Exposed persons may also occupy several different areas over the course of any given day, some of which may contribute far more significantly to the total radiation dose they incur. Methods of calculating annual doses from measured or calculated dose rates are also described in detail in Appendix B of this guide.
3.2.1.2 Dose Estimates for Positron Emission Tomography (PET) Applications
The basic approach to Positron Emission Tomography (PET) shielding design is similar to that for conventional diagnostic nuclear medicine described in subsection 3.2.1.1, Dose Estimates for Conventional Diagnostic Nuclear Medicine—A Five-Step Method. The significant difference is in the details; for example, the thickness of shielding required, due to the higher energy 511 keV annihilation gammas that are produced.
In such cases, the use of lead may be impractical because of weight and structural considerations. Concrete, either in the form of poured slabs or solid concrete block, is generally a more viable solution to PET shielding issues. The choice of shielding materials is ultimately left to the licensee.
The Medical Physics periodical (33, 1; January 2006) provides useful technical information and guidance on shielding requirements and dose estimates specifically related to PET operations [1].
3.2.1.3 Dose Estimates for In-Patient 131I Therapy Applications
There is very little difference between conventional diagnostic nuclear medicine dose estimates and those for in-patient nuclear medicine treatments, such as 131I thyroid cancer treatment. However, the patient is typically isolated in a dedicated treatment room on one of the wards.
The basic approach to 131I in-patient therapy room shielding calculations is similar to that for conventional diagnostic nuclear medicine described in subsection 3.2.1.1, Dose Estimates for Conventional Diagnostic Nuclear Medicine—A Five-Step Method. The significant difference is that, as a condition of the licence, the design must be such that the dose rate in occupied areas around the treated patient’s room does not exceed 2.5 µSv/hour or that other patients do not receive a dose in excess of 500 µSv per hospital stay.
3.2.2 Dose Estimates for High and Containment Level Laboratories
For high and containment level laboratories, doses should also be considered at the planning stage. In this case, localized shielding is typically used to ensure dose rates in the surrounding areas are acceptable. The main sources of radiation and the shielding materials should be considered, and resulting dose rates should be provided (by measurement or by calculation). Occupancy of persons in adjacent or nearby areas should be considered and resulting annual doses determined. The intended use of procedural and work practice controls should also be considered and explained.
If specific dose estimates are required, CNSC staff may request additional information upon submission of the application.
3.2.3 Dose Estimates for Nuclear Substance Laboratories in Veterinary Nuclear Medicine
Dose estimates for veterinary nuclear medicine are very similar to dose estimates for conventional diagnostic nuclear medicine. Therefore, the approach to veterinary nuclear medicine shielding calculations is the same as that for conventional diagnostic nuclear medicine (see subsection 3.2.1.1, Dose Estimates for Conventional Diagnostic Nuclear Medicine—A Five-Step Method).
Appendix A: Dose Conversion Factors (DCF) and Annual Limits on Intake (ALI) for Common Nuclear Substances
| Nuclear Substance |
DCF (Sv/Bq) Inhalation |
ALI (Bq) Inhalation |
DCF (Sv/Bq) Ingestion |
ALI (Bq) Ingestion |
|---|---|---|---|---|
| Actinium 227 (227Ac) | 6.3 × 10-4 | 3.2 × 101 | 1.1 × 10-6 | 1.8 × 104 |
| Aluminum 26 (26Al) | 1.4 × 10-8 | 1.4 × 106 | 3.5 × 10-9 | 6.0 × 106 |
| Americium 241 (241Am) | 2.7 × 10-5 | 7.4 × 102 | 2.0 × 10-7 | 1.0 × 105 |
| Antimony 124 (124Sb) | 4.7 × 10-9 | 4.3 × 106 | 2.5 × 10-9 | 8.0 × 106 |
| Arsenic 74 (74As) | 1.8 × 10-9 | 1.1 × 107 | 1.3 × 10-9 | 1.5 × 107 |
| Barium 133 (133Ba) | 1.8 × 10-9 | 1.1 × 107 | 1.0 × 10-9 | 2.0 × 107 |
| Barium 140 (140Ba) | 1.6 × 10-9 | 1.3 × 107 | 2.5 × 10-9 | 8.0 × 106 |
| Beryllium 7 (7Be) | 4.6 × 10-11 | 4.3 × 108 | 2.8 × 10-11 | 7.1 × 108 |
| Beryllium 10 (10Be) | 1.9 × 10-9 | 1.1 × 106 | 1.1 × 10-9 | 1.8 × 107 |
| Bismuth 207 (207Bi) | 3.2 × 10-9 | 6.3 × 106 | 1.3 × 10-9 | 1.5 × 107 |
| Bismuth 210 (210Bi) | 6.0 × 10-8 | 3.3 × 105 | 1.3 × 10-9 | 1.5 × 107 |
| Bromine 82 (82Br) | 8.8 × 10-10 | 2.3 × 107 | 5.4 × 10-10 | 3.7 × 107 |
| Cadmium 109 (109Cd) | 9.6 × 10-9 | 2.1 × 106 | 2.0 × 10-9 | 1.0 × 107 |
| Calcium 45 (45Ca) | 2.3 × 10-9 | 8.7 × 106 | 7.6 × 10-10 | 2.6 × 107 |
| Californium 252 (252Cf) | 1.3 × 10-5 | 1.5 × 103 | 9.0 × 10-8 | 2.2 × 105 |
| Carbon 11 (11C) | 2.2 × 10-12 | 9.1 × 109 | 2.4 × 10-11 | 8.3 × 108 |
| Carbon 14 * (14C) | 2.0 × 10-11 | 1.0 × 109 | 5.8 × 10-10 | 3.4 × 107 |
| Cerium 141 (141Ce) | 3.1 × 10-8 | 6.5 × 106 | 7.1 × 10-10 | 2.8 × 107 |
| Cerium 144 (144Ce) | 2.9 × 10-8 | 6.9 × 105 | 5.2 × 10-9 | 3.8 × 106 |
| Cesium 134 (134Cs) | 9.6 × 10-9 | 2.1 × 106 | 1.9 × 10-8 | 1.1 × 106 |
| Cesium 137 (137Cs) | 6.7 × 10-9 | 3.0 × 106 | 1.3 × 10-8 | 1.5 × 106 |
| Chlorine 36 (36Cl) | 5.1 × 10-9 | 3.9 × 106 | 9.3 × 10-10 | 2.2 × 107 |
| Chromium 51 (51Cr) | 3.6 × 10-11 | 5.6 × 108 | 3.8 × 10-11 | 5.3 × 108 |
| Cobalt 57 (57Co) | 6.0 × 10-10 | 3.3 × 107 | 2.1 × 10-10 | 9.5 × 107 |
| Cobalt 58 (58Co) | 1.7 × 10-9 | 1.2 × 107 | 7.4 × 10-10 | 2.7 × 107 |
| Cobalt 60 (60Co) | 1.7 × 10-8 | 1.2 × 106 | 3.4 × 10-9 | 5.9 × 106 |
| Copper 64 (64Cu) | 1.5 × 10-10 | 1.3 × 108 | 1.2 × 10-10 | 1.7 × 108 |
| Copper 67 (67Cu) | 5.8 × 10-10 | 3.4 × 107 | 3.4 × 10-10 | 5.9 × 107 |
| Curium 244 (244Cm) | 1.7 × 10-5 | 1.2 × 103 | 1.2 × 10-7 | 1.7 × 105 |
| Fluorine 18 (18F) | 9.3 × 10-11 | 2.2 × 108 | 4.9 × 10-11 | 4.1 × 108 |
| Gadolinium 153 (153Gd) | 2.5 × 10-9 | 8.0 × 106 | 2.7 × 10-10 | 7.4 × 107 |
| Gallium 67 (67Ga) | 2.8 × 10-10 | 7.1 × 107 | 1.9 × 10-10 | 1.1 × 108 |
| Gallium 68 (68Ga) | 8.1 × 10-11 | 2.5 × 108 | 1.0 × 10-10 | 2.0 × 108 |
| Germanium 68 (68Ge) | 7.9 × 10-9 | 2.5 × 106 | 1.3 × 10-9 | 1.5 × 107 |
| Gold 198 (198Au) | 1.1 × 10-9 | 1.8 × 107 | 1.0 × 10-9 | 2.0 × 107 |
| Hydrogen 3 (HT) (3H) | 2.0 × 10-15 | 1.0 × 1013 | -- | -- |
| Hydrogen 3 (HTO) ** (3H) | 2.0 × 10-11 | 1.0 × 109 | 2.0 × 10-11 | 1.0 × 109 |
| Hydrogen 3 (OBT) † (3H) | 4.1 × 10-11 | 4.9 × 108 | 4.2 × 10-11 | 4.8 × 108 |
| Indium 111 (111In) | 3.1 × 10-10 | 6.5 × 107 | 2.9 × 10-10 | 6.9 × 107 |
| Indium 113m (113mIn) | 3.2 × 10-11 | 6.3 × 108 | 2.8 × 10-11 | 7.1 × 108 |
| Indium 114m (114mIn) | 1.1 × 10-8 | 1.8 × 106 | 4.1 × 10-9 | 4.9 × 106 |
| Iodine 123 (123I) | 2.1 × 10-10 | 9.5 × 107 | 2.1 × 10-10 | 9.5 × 107 |
| Iodine 124 (124I) | 1.2 × 10-8 | 1.7 × 106 | 1.3 × 10-8 | 1.5 × 106 |
| Iodine 125 (125I) | 1.4 × 10-8 | 1.4 × 106 | 1.5 × 10-8 | 1.3 × 106 |
| Iodine 129 (129I) | 9.6 × 10-8 | 2.1 × 105 | 1.1 × 10-7 | 1.8 × 105 |
| Iodine 131 (131I) | 2.0 × 10-8 | 1.0 × 106 | 2.2 × 10-8 | 9.1 × 105 |
| Iodine 132 (132I) | 3.1 × 10-10 | 6.5 × 107 | 2.9 × 10-10 | 6.9 × 107 |
| Iridium 192 (192Ir) | 4.9 ×10-9 | 4.1 × 106 | 1.4 × 10-9 | 1.4 × 107 |
| Iron 55 (55Fe) | 9.2 × 10-10 | 2.2 × 107 | 3.3 × 10-10 | 6.1 × 107 |
| Iron 59 (59Fe) | 3.2 × 10-9 | 6.3 × 106 | 1.8 × 10-9 | 1.1 × 107 |
| Krypton 85 (gas) Bq/m3 ‡ (85Kr) | 2.2 × 10-11 | 9.1 × 108 | -- | -- |
| Lanthanum 140 (140La) | 1.5 × 10-9 | 1.3 × 107 | 2.0 × 10-9 | 1.0 × 107 |
| Lead 210 (210Pb) | 1.1 × 10-6 | 1.8 × 104 | 6.8 × 10-7 | 2.9 × 104 |
| Magnesium 28 (28Mg) | 1.7 × 10-9 | 1.2 × 107 | 2.2 × 10-9 | 9.0 × 106 |
| Manganese 54 (54Mn) | 1.2 × 10-9 | 1.7 × 107 | 7.1 × 10-10 | 2.8 × 107 |
| Manganese 56 (56Mn) | 2.0 × 10-10 | 1.0 × 108 | 2.5 × 10-10 | 8.0 × 107 |
| Mercury 194 (organic) (194Hg) | 1.9 × 10-8 | 1.1 × 106 | 5.1 × 10-8 | 3.9 × 105 |
| Mercury 197 (organic) (197Hg) | 8.5 × 10-11 | 2.4 × 108 | 1.7 × 10-10 | 1.2 × 108 |
| Mercury 197 (inorganic) (197Hg) | 2.8 × 10-10 | 7.1 × 107 | 2.3 × 10-10 | 8.7 × 107 |
| Mercury 203 (organic) (203Hg) | 7.5 × 10-10 | 2.7 × 107 | 1.9 × 10-9 | 1.1 × 107 |
| Mercury 203 (inorganic) (203Hg) | 1.9 × 10-9 | 1.1 × 107 | 5.4 × 10-10 | 3.7 × 107 |
| Molybdenum 99 (99Mo) | 1.1 × 10-9 | 1.8 × 107 | 1.2 × 10-9 | 1.7 × 107 |
| Nickel 63 (63Ni) | 5.2 × 10-10 | 3.8 × 107 | 1.5 × 10-10 | 1.3 × 108 |
| Niobium 95 (95Nb) | 1.3 × 10-9 | 1.5 × 107 | 5.8 × 10-10 | 3.4 × 107 |
| Phosphorus 32 (32P) | 2.9 × 10-9 | 6.9 × 106 | 2.4 × 10-9 | 8.3 × 106 |
| Phosphorus 33 (33P) | 1.3 × 10-9 | 1.5 × 107 | 2.4 × 10-10 | 8.3 × 107 |
| Plutonium 239 (239Pu) | 3.2 × 10-5 | 6.3 × 102 | 2.5 × 10-7 | 8.0 × 104 |
| Plutonium 240 (240Pu) | 3.2 × 10-5 | 6.3 × 102 | 2.5 × 10-7 | 8.0 × 104 |
| Polonium 209 (209Po) | 2.3 × 10-6 | 8.8 × 103 | 3.0 × 10-7 | 6.6 × 104 |
| Polonium 210 (210Po) | 2.2 × 10-6 | 9.1 × 103 | 2.4 × 10-7 | 8.3 × 104 |
| Potassium 42 (42K) | 2.0 × 10-10 | 1.0 × 108 | 4.3 × 10-10 | 4.7 × 107 |
| Promethium 147 (147Pm) | 3.5 × 10-9 | 5.7 × 106 | 2.6 × 10-10 | 7.7 × 107 |
| Protactinium 233 (233Pa) | 3.2 × 10-9 | 6.3 × 106 | 8.7 × 10-10 | 2.3 × 107 |
| Radium 223 (223Ra) | 5.7 × 10-6 | 3.5 × 103 | 1.0 × 10-7 | 2.0 × 105 |
| Radium 226 (226Ra) | 2.2 × 10-6 | 9.1 × 103 | 2.8 × 10-7 | 7.1 × 104 |
| Rhenium 186 (186Re) | 1.2 × 10-9 | 1.7 × 107 | 1.5 × 10-9 | 1.3 × 107 |
| Rhenium 188 (188Re) | 7.4 × 10-10 | 2.7 × 107 | 1.4 × 10-9 | 1.4 × 107 |
| Rubidium 86 (86Rb) | 1.3 × 10-9 | 1.5 × 107 | 2.8 × 10-9 | 7.1 × 106 |
| Ruthenium 103 (103Ru) | 2.2 × 10-9 | 9.1 × 106 | 7.3 × 10-10 | 2.7 × 107 |
| Scandium 46 (46Sc) | 4.8 × 10-9 | 4.2 × 106 | 1.5 × 10-9 | 1.3 × 107 |
| Selenium 75 (75Se) | 1.7 × 10-9 | 1.2 × 107 | 2.6 × 10-9 | 7.7 × 106 |
| Silicon 31 (31Si) | 1.1 × 10-10 | 1.8 × 108 | 1.6 × 10-10 | 1.3 × 108 |
| Silicon 32 (32Si) | 5.5 × 10-8 | 3.6 × 105 | 5.6 × 10-10 | 3.5 × 107 |
| Silver 110m (110mAg) | 7.3 × 10-9 | 2.7 × 106 | 2.8 × 10-9 | 7.1 × 106 |
| Sodium 22 (22Na) | 2.0 × 10-9 | 1.0 × 107 | 3.2 × 10-9 | 6.3 × 106 |
| Sodium 24 (24Na) | 5.3 × 10-10 | 3.8 × 107 | 4.3 × 10-10 | 4.7 × 107 |
| Strontium 85 (85Sr) | 6.4 × 10-10 | 3.1 × 107 | 5.6 × 10-10 | 3.6 × 107 |
| Strontium 89 (89Sr) | 5.6 × 10-9 | 3.6 × 106 | 2.6 × 10-9 | 7.7 × 106 |
| Strontium 90 (90Sr) | 7.7 × 10-8 | 2.6 × 105 | 2.8 × 10-8 | 7.1 × 105 |
| Sulphur 35 (inorganic) (35S) | 1.1 × 10-9 | 1.8 × 107 | 1.9 × 10-10 | 1.1 × 108 |
| Sulphur 35 (organic v) (35S) | 1.2 × 10-10 | 1.7 × 108 | 7.7 × 10-10 | 2.6 × 107 |
| Technetium 99m (99mTc) | 2.9 × 10-11 | 6.9 × 108 | 2.2 × 10-11 | 9.1 × 108 |
| Technetium 99 (99Tc) | 3.2 × 10-9 | 6.3 × 106 | 7.8 × 10-10 | 2.6 × 107 |
| Thallium 201 (201Tl) | 7.6 × 10-11 | 2.6 × 108 | 9.5 × 10-11 | 2.1 × 108 |
| Thallium 204 (204Tl) | 6.2 × 10-10 | 3.2 × 107 | 1.3 × 10-9 | 1.5 × 107 |
| Thorium 228 (228Th) | 3.2 × 10-5 | 6.3 × 102 | 6.9 × 10-8 | 2.9 × 105 |
| Thorium 229 (229Th) | 6.9 × 10-5 | 2.9 × 102 | 4.8 × 10-7 | 4.2 × 104 |
| Thorium 230 (230Th) | 2.8 × 10-5 | 7.1 × 102 | 2.1 × 10-7 | 9.5 × 104 |
| Tin 113 (113Sn) | 1.9 × 10-9 | 1.1 × 107 | 7.3 × 10-10 | 2.7 × 107 |
| Uranium (natural) †† | 6.3 × 10-6 | 3.2 × 103 | 9.5 × 10-9 | 2.1 × 106 |
| Uranium (depleted) †† | 5.9 × 10-6 | 3.4 × 103 | 1.1 × 10-8 | 1.9 × 106 |
| Uranium 232 (232U) †† | 2.6 × 10-5 | 7.7 × 102 | 3.3 × 10-7 | 6.1 × 104 |
| Uranium 233 (233U) †† | 6.9 × 10-6 | 2.9 × 103 | 5.0 × 10-8 | 4.0 × 105 |
| Uranium 235 (235U) †† | 6.1 × 10-6 | 3.3 × 103 | 4.6 × 10-8 | 4.3 × 105 |
| Uranium 236 (236U) †† | 6.3 × 10-6 | 3.2 × 103 | 4.6 × 10-8 | 4.3 × 105 |
| Uranium 238 (238U) †† | 5.7 × 10-6 | 3.5 × 103 | 4.4 × 10-8 | 4.5 × 105 |
| Xenon 133 (gas) Bq/cm3 ‡ (133Xe) | 1.2 × 10-10 | 6.7 × 105 | -- | -- |
| Xenon 135 (gas) Bq/cm3 ‡ (135Xe) | 9.6 × 10-10 | 8.3 × 104 | -- | -- |
| Yttrium 87 (87Y) | 5.3 × 10-10 | 3.8 × 107 | 5.5 × 10-10 | 3.6 × 107 |
| Yttrium 90 (90Y) | 1.7 × 10-9 | 1.2 × 107 | 2.7 × 10-9 | 7.4 × 106 |
| Zinc 65 (65Zn) | 2.8 × 10-9 | 7.1 × 106 | 3.9 × 10-9 | 5.1 × 106 |
* CO2 value from ICRP-based data published from 1955-1970. New data (1990-2000) and revision of the model
(2004) recommend higher dose coefficient. Revised 14CO2 dose coefficient from
Leggett, R.W., Radiation Protection Dosimetry Vol. 208, pp. 203-213 (2004).
** Hydrogenated Tritium Oxide (HTO), also referred to as “tritiated water”
ICRP DCF is 1.8E-11; value used here is from Health Canada 83-EHD-87 (1983) and RSP-182B (2004).
† Organically Bound Tritium (OBT)
‡ The concentration equivalent of 20 mSv per year (assuming 250 working days and 8-hour workday).
†† Type S (slow), insoluble compounds
Appendix B: Calculating Dose Estimates
The following example demonstrates one method (as introduced in subsection 3.2.1.1, Dose Estimates for Conventional Diagnostic Nuclear Medicine—A Five-Step Method), for estimating the radiation doses from nuclear medicine operations. The same approach can be used to estimate the shielding based on dose targets.
Appendix B1: Sample Calculation for Dose Estimates for Nuclear Medicine Rooms
Using the method outlined in subsection 3.2.1.1, the following approach can be used to estimate the doses to persons (other than the patient) in and around a nuclear medicine room.
Step 1) Facility Layout
Figure B1 shows a hypothetical nuclear medicine department layout. Dimensions and basic shielding details are shown. Key locations where nuclear substances and nuclear medicine patients will be present for significant periods of time over the course of the workday are identified using letters A to D2.
Step 2) Estimating Workload
For any given nuclear medicine facility, several different gamma emitting nuclear substances can be identified that are used regularly (e.g., 51Cr, 67Ga, 99mTc, 111In, 123I, 131I and 201Tl). It is unlikely that all of the nuclear substances will be used or will contribute significantly to the annual dose at a particular location. Rather, it is likely that only one or two nuclear substances and procedures will be of importance.
Example:
Assume that the nuclear medicine department shown in Figure 1 primarily performs three types of outpatient diagnostic procedures: cardiac analysis, diagnostic bone scans and thyroid uptake analysis. The typical daily workload and details of the nuclear substances and activities used are presented in Table B1. The annual number of procedures performed is estimated from the daily workload by assuming five days of operation per week (procedures are not done on the weekends), 50 weeks per year.
Figure B1: Hypothetical Nuclear Medicine Department Layout
.png/object)
| Procedure | Nuclear Substance | Number of Procedures per Year | Average Procedure Duration | Average Activity Per Treatment | (No. of Proc.) x (Duration) x (Activity) |
|---|---|---|---|---|---|
| Cardiac analysis | 99mTc | 1200 | 1 ½ h * |
370 MBq (rest)* 1100 MBq (stress)* |
259,000 MBq-h* 1,210,000 MBq-h* |
| Bone scans | 99mTc | 500 | ¾ h | 800 MBq | 300,000 MBq-h |
| Thyroid uptake | 131I | 100 | ½ h | 0.37 MBq | 18.5 MBq-h |
* Assumes 35 minutes for rest test and 55 minutes for stress test (90 minutes total, or 1 ½ hours)
From the final column, it is reasonable to assume that, for this example, the radiation doses incurred by staff or the general public as a result of thyroid uptake procedures are negligible in comparison with cardiac analysis or bone scans and can be omitted from the dose estimation. However, all types of procedures, total number of patients and average activities should be provided to the CNSC and those used in the assessment should be justified.
Step 3) Occupancy Review
To begin, it must be determined who is exposed to radiation as a consequence of the operation of the nuclear medicine department. For compliance with the Radiation Protection Regulations, these persons may be considered as either NEWs or non-NEWs.
According to the NSCA, a NEW is a person who is required, in the course of the person’s business or occupation in connection with a nuclear substance or nuclear facility, to perform duties in such circumstances that there is a reasonable probability that the person may receive a dose of radiation that is greater than the prescribed limit for the general public, which is 1 mSv. For example, nuclear medicine technologists are usually designated as NEWs.
Non-NEWs may be staff members or members of the general public, and as such are subject to an annual effective dose limit of 1 mSv.
Assessing the doses received by every individual from every possible source is impractical, so the evaluation may be simplified by evaluating the proximity, frequency, and duration of exposure for persons in each group to establish the most exposed persons. Only these “worst case” exposures within each group should be evaluated, as all other persons within each group can be safely assumed to receive lesser doses.
The final stage of the occupancy review determines:
- Where the nuclear substances and nuclear medicine patients are present (see Figure B1, locations A, B, C, D1, and D2) and for how long; and
- Where the most exposed individuals (other than the patient undergoing the nuclear medicine procedure) are present and for how long.
For each location in and around the facility where a significant contribution to the total dose received by a person would be expected, the dose to each representative person, assuming an appropriate occupancy factor, should be determined. The presence of NEWs, non-NEWs, or both, at these locations should be specified. If an individual occupies several of these locations, the dose from all locations should be totalled (this scenario should be considered when assigning occupancy factors).
If occupancy factors are not known, NCRP 151 provides guidance on occupancy factors. NCRP 151 also addresses issues of ventilation, electrical outlets, and fixture design considerations for radiation protected facilities.[4]
Example:
For the purposes of this example, assume the following:
- There is one full time receptionist for the nuclear medicine department who spends most of their time in the reception office. The same is true for the adjacent outpatient clinic.
- Other ancillary staff, such as cleaning and maintenance staff, are present only infrequently, with restricted access to areas in which nuclear substances are used and with minimal direct exposure to injected patients or radiopharmaceuticals.
- Members of the general public who accompany the patients undergoing nuclear medicine procedures do so a maximum of a few times per year.
- Physicians working in the adjacent outpatient clinic spend approximately one half of their time in the examining rooms immediately adjacent to the camera suites and stress testing room.
- The clinic is a single story building, built on grade, so there is no occupancy below and very minimal occupancy above (e.g., during roof repairs).
For this example, we assume that persons (other than the patient) will occupy the following locations: the corridor, the office, the camera room(s), the exam rooms in the neighbouring clinic, and the reception area. These key locations cover areas of occupancy of technicians (NEWs) and non-NEWs, including the physician in the adjoining clinic. Other locations may also need to be considered—the locations used in this example are for illustrative purposes. The complete example in this guide is worked out only for the reception area/receptionist. The same approach would be used for the other locations or other representative individuals.
The key parameters needed to estimate the total annual doses are listed in Table B2.
| Non-NEW | NEW | Important Location(s) Occupied | Source Location(s) Making Significant Contribution to Dose | Occupancy Factor (T) At Each Location Occupied | Rationale/Comment |
|---|---|---|---|---|---|
| Yes | Yes | Corridor | A, B, C, D1, D2 | 1/16 | |
| No | Yes | Office | A, B, C, D1, D2 | 1/4 | |
| No | Yes | Camera Room 1 or Camera Room 2 | D1 or D2 | 1 | Although procedures will be split between Camera Rooms 1 and 2, when evaluating the dose to a technologist, it can be assumed that all of the procedures are performed in one room, since this will not alter the total dose received by the technologist. |
| Yes | No | Nuclear Medicine Reception | A, B, D1, D2 | 1 | C need not be considered since radiation emitted from injected patients in these rooms must pass through multiple shielded walls to reach the reception area. |
| Yes | No | Exam Room 2 | C, D1, D2 | 1/2 |
An occupancy factor of 1/2 is used because it was stated that each physician spends approximately 1/2 their time in the Exam Rooms. A physician may be present in any of Exam Rooms 1, 2 or 3. The central room, Exam 2, is reasonably representative of their average location. Source locations A and B are distant from the Exam Rooms and are doubly shielded by the lead lining of the intervening Stress Test and Camera Rooms and thus will make a negligibly small contribution to the dose in comparison with source locations C, D1, and D2. |
Step 4) Dose Rate Calculations
The following approach assumes the source/patient can be approximated as a point source. For most distances, the point source is a sufficiently accurate representation. In addition, at distances greater than 1 meter, assuming point source geometry is conservative compared to other viable geometrics such as a volumetric source. The choice of source geometry is left to the discretion of the applicant, but the method for estimation must be clearly indicated.
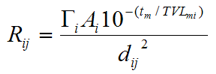
A general formula for performing dose rate calculations for a point source is:
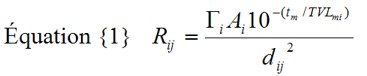
| Where: | ||
|---|---|---|
| Rij | is the dose rate produced by nuclear substance i at location j | (μSv h-1) |
| Γi | is the specific gamma ray constant for nuclear substance i | (μSv h-1 MBq-1 m2) |
| Ai | is the activity of nuclear substance i | (MBq) |
| dij | is the distance between nuclear substance i and location j | (m) |
| tm | is the thickness of shielding material m in any shielded barrier between nuclear substance i and location j | (mm) |
| TVLmi | is the “Tenth Value Layer” thickness of material m for nuclear substance i (i.e., the thickness of material m that would be required to reduce the photon radiation dose rate produced by nuclear substance i to 1/10th of its initial value) | (mm) |
Specific gamma ray constants are typically defined in terms of the dose rate produced (e.g., μSv h-1) at one meter from the source, per unit of source activity (e.g., MBq-1). When performing dose rate calculations, care must be taken to ensure the consistency of units between Rij, Γi and Ai. Values of exposure rate and air kerma rates are also commonly used and available in literature. These values should be converted to values of dose rate.
Tenth value layer (TVL) thicknesses for common gamma-emitting nuclear substances and various shielding materials are available from a number of different sources [5]. Diagnostic nuclear medicine rooms are typically shielded using commercially available lead sheeting, with normal thicknesses varying from 0.8 mm (1/32 inch) to 3.2 mm (1/8 inch). For poly-energetic sources, the “first” broad beam TVL thickness may be much smaller than subsequent TVLs due to the selective absorption of low energy photons via photoelectric interactions. This effect is commonly referred to as “radiation hardening” or “beam hardening”. For this reason, care must be taken when evaluating transmission through barriers greater than 1 TVL thick for nuclear substances such as 67Ga, 111In, 123I, 131I, or 201Tl.
Example:
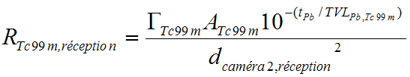
Table B3 summarizes the parameters required to perform the dose rate estimates for the receptionist. The distances dij were measured directly from Figure B1. Lead thicknesses are based on the assumption that all interior walls of Stress Testing, Camera Room 1, Camera Room 2 and the “hot” post-injection waiting room are lined with 1.6 mm (1/16 inch) lead. All other interior walls are assumed to be constructed of ordinary drywall (gypsum board) and to provide minimal attenuation.
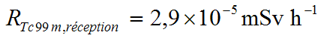
The final column of Table B3 lists the calculated dose rates at the reception desk resulting from bone scan and cardiac stress test procedures. A sample calculation for one representative source location (D2) and procedure (imaging after stress testing) is given below:
| Source i Location |
Distance dij (m) |
Lead Thickness tm (mm) |
Activity Ai (MBq) which may temporarily be present at each source location due to each procedure | Dose rate Rij (mSv h-1) at occupied location j while source activity Ai is present at each source location | ||||
|---|---|---|---|---|---|---|---|---|
| Cardiac (rest) | Cardiac (stress) | Bone Scan | Cardiac (rest) | Cardiac (stress) | Bone scan | |||
| A | 10 | 0 | 370 | 1470 | 800 | 7.3 × 10-5 | 2.9 × 10-4 | 1.6 × 10-4 |
| B | 13 | 1.6 | 370 | 1470 | 800 | 1.1 × 10-6 | 4.3 × 10-6 | 2.3 ×10-6 |
| C | As noted in Table B2, C need not be considered since radiation emitted from injected patients in these rooms must pass through multiple shielded walls to reach the reception area. | |||||||
| D1 | 9 | 3.2 | 370 | 1470 | 800 | 5.7 × 10-8 | 2.3 × 10-7 | 1.2 × 10-7 |
| D2 | 5 | 1.6 | 370 | 1470 | 800 | 7.3 × 10-6 | 2.9 × 10-5 | 1.6 × 10-5 |
Using equation {1}:
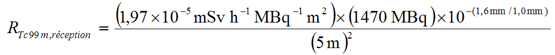
For simplicity, there was no correction for the decay (radiological or biological) of 99mTc in this
calculation.
3 NCRP 124 [5]; air kerma values were converted to dose using NIST values [6] for mass energy absorption coefficients.
4 NCRP 124 [5]; broad beam HVLs were provided and converted to TVLs.
Step 5) Annual Dose Calculations
The total dose estimated per year, for any given combination of procedure, source location, occupied location and exposed person, is given by the product of: the total number of procedures performed per year (N, see Table B1); the occupancy factor for the exposed person and occupied location (T, see Table B2); the dose rate (Rij, see Table B3); and the duration of time (Si) the source/injected patient is present at the designated source location (in hours). The annual dose (Dij) is then:
Equation {2} Dij = N × T × Rij × Si
Example:
Table B4 summarizes the parameters required to perform the dose estimates for the example. Estimated total procedure times were given in Table B1. These are broken down into the approximate times the source/patient spends at each key location (Si) in Table B4.
| For example, cardiac stress testing was estimated to require 1½ hours. This time has been divided into: | |
|---|---|
| 2 minutes for the rest test injection | 0.033 h |
| 20 minutes in the post-injection waiting room | 0.33 h |
| 15 minutes scanning in either camera room | 0.25 h |
| 2 minutes for the stress test injection | 0.033 h |
| 20 minutes in the waiting room | 0.33 h |
| 15 minutes in the treadmill room | 0.25 h |
| 15 minutes scanning in either camera room | 0.25 h |
| Total: | 1.48 h |
Table B4: Annual Dose Calculations
The last column of Table B4 lists the calculated annual doses to the reception area (for the receptionist), for both the bone scan and cardiac procedures (note that for the reception area, the exposure from the patient in the treadmill room (C) can be neglected as was noted in Tables B2 and B3). A sample calculation for one representative source location (D2) and one part of the procedure (imaging after stress testing) is given below:
Using equation {2}, this gives:
Appendix B2: Conclusion
The annual dose to the receptionist and reception area, assuming 100% occupancy, is less than 50 µSv.
To complete the dose assessment, the annual doses would be estimated for other staff and members of the general public, other than the patient, who are in and around the nuclear medicine rooms in the facility. The CNSC may consider that an ALARA assessment is not required when individual occupational doses are unlikely to exceed 1 mSv per year, when the dose to individual members of the public is unlikely to exceed 50 µSv per year, and when the annual collective dose (both occupational and public) is unlikely to exceed 1 person-Sv (as recommended in CNSC document G-129 rev 1, Keeping Radiation Doses and Exposures ALARA, as amended from time to time).
Appendix C: Design Assessment Form
The following pages may be completed and submitted as part of the licence application. Retain a copy for your records.
This Design Assessment Form (DAF) provides guidance and recommendations for best laboratory practices [7,8,9,10]. Alternative design features that provide an equivalent degree of safety will be considered. For alternative design features, please include a justification for the variance as a separate attachment.
Design Assessment Form for Nuclear Substance Laboratories and Nuclear Medicine Rooms
The following pages may be detached from the guide and mailed in as part of the licence application.
(Note: A separate form should be completed for each room, unless their design, their functions and classifications are identical or if they are similar).
Every effort should be made to meet the guidelines set out in this form as they are all good laboratory practices. Alternatives that provide an equivalent degree of safety will be reviewed.
High level and containment level laboratories and nuclear medicine rooms have additional considerations and certain items (i.e., dose estimates) are related only to those classifications. Additional information may be requested by the CNSC after the initial assessment.
| B | Finishing and Fixtures (for use and storage areas) | Yes | No | Justification for variance included as separate attachment |
|---|---|---|---|---|
| B1 | Flooring will have an impervious, chemical resistant, washable surface. Carpeting will not be used. | |||
| B2 | Either all joints in the flooring material will be sealed, or the flooring will be a one-piece design. | |||
| B3 | Flooring will have a strippable coating for easier clean-up if contaminated. | |||
| B4 | Flooring will be coved up walls and cabinets to prevent spills from penetrating underneath them. | |||
| B5 | Work surfaces will have a smooth, impervious, washable, and chemical-resistant finish. | |||
| B6 | Either all joints on work surfaces will be sealed, or bench tops will have a seamless one-piece design. | |||
| B7 | The countertop will include a lip to prevent run-off onto the floor. If the countertop abuts a wall, it will either be coved or have a back-splash against the wall. | |||
| B8 | All cupboards and shelving where nuclear substances may be stored will have a smooth, impervious, washable, and chemical-resistant finish. | |||
| B9 | Walls will be finished with a smooth and washable surface and the joints will be sealed where applicable, for easier clean-up if contaminated due to backspray from a vial or some other such event. | |||
| B10 | The ceiling will be finished with a smooth and washable surface and the joints will be sealed where applicable, for easier clean-up if contaminated due to backspray from a vial or some other such event. | |||
| B11 | If necessary, work surfaces will be reinforced to bear the (possibly considerable) weight of any shielding material that may be placed on the work surface. | |||
| B12 | A separate hand washing sink and a wash-up/disposal sink will be provided. | |||
| B12 | Hand washing sinks will be close to the room’s entrance, to encourage hand washing on the way out of the room. | |||
| B14 | Sinks will be made of material that is readily decontaminated. | |||
| B15 | Each sink will have an overflow outlet. | |||
| B16 | Faucets will be operated by means not requiring direct hand contact. | |||
| B17 | An emergency eye-wash station will be provided in the room or in close proximity to the room. | |||
| B18 | An emergency shower will be provided in close proximity to the room, for use in the event of major personnel contamination. | |||
| B19 | Emergency lighting will be provided within the room. | |||
| B20 | Facilities for storing outer garments and personal items will be provided outside the room. | |||
| B21 | Coat hooks will be provided within the room, close to the room entrance, to encourage personnel to remove potentially-contaminated lab coats before leaving the room. | |||
| C | Plumbing | Yes | No | Justification for variance included as separate attachment |
| C1 | Drains that may carry radioactive material from the area will go directly to the main building sewer or to the facility’s controlled active liquid waste system. | |||
| C2 | Drains from the room will be identified on plans supplied to maintenance personnel. | |||
| C3 | Drains will be constructed of chemical-resistant material. | |||
| C4 | A backflow protection device will be in place to prevent potentially contaminated water from entering the public water system. | |||
| C5 | Drain lines that may carry radioactive material will be marked at 3 meter intervals with the radiation warning symbol to indicate the possibility of contamination. | |||
| C6 | Sink drain traps will be accessible for monitoring. | |||
| C7 | Faucets with vacuum or cooling line attachments will include backflow protection devices. | |||
| D | Security | Yes | No | Justification for variance included as separate attachment |
| D1 | An access control system (key, keypad, key fob, other) will be in place to ensure that only authorized users can enter the restricted room. | |||
| D2 | The room will be equipped with lockable doors that will remain closed and locked whenever nuclear substances and radiation devices are present in the room and the room is unoccupied. | |||
| D3 | Any windows on the ground floor will be secured to prevent unauthorized access to the room. | |||
| D4 | If the room is to be shared with workers not authorized to use nuclear substances, a secondary lockable storage area (refrigerator, freezer, cupboard) will be provided within the room. | |||
| E | Ventilation | Yes | No | Justification for variance included as separate attachment |
|
Note: This section is to be completed only if volatile nuclear substances are to be used or stored, or if aerosols or gases are likely to be produced. If Biological Safety Cabinets, glove boxes, or “hot cells” are deemed necessary for the work being performed, detailed information should be provided about these systems. |
||||
| E1 | The room will be at negative pressure with the surrounding area (unless the room will be used as a clean or sterile room). Air flow will always be from the area of low radiation. For clean or sterile rooms, an anteroom may be required. | |||
| E2 | General laboratories will have a minimum of 6 air changes per hour. | |||
| E3 | The fume hood will be selected based on its adequacy for the intended work. | |||
| E4 | Air vented through the fume hood will be vented without recirculation. | |||
| E5 | Fume hoods will be located away from areas of air currents or turbulence (high traffic areas, doors, operable windows, air supply diffusers). | |||
| E6 | Fume hoods will not be located adjacent to a single means of access to an exit, due to possible volatility of the fume hood contents. | |||
| E7 | To avoid interference, supply air vents will be installed away from, or directed away from, fume hoods. | |||
| E8 | If a fume hood is the sole means of room air exhaust, a bypass will be installed to ensure ventilation when the sash is closed. | |||
| E9 | The fume hood will be constructed of smooth, impervious, washable, and chemical-resistant material. | |||
| E10 | The fume hood will have a means of containing a minor spill. | |||
| E11 | The interior of the fume hood will have coved corners for easy decontamination and clean-up. | |||
| E12 | The work surface of the fume hood will be reinforced to bear the weight of any shielding material that is required. | |||
| E13 | Fume hoods will be labelled to show which fan or ventilation system they are connected to. | |||
| E14 | The face velocity of the fume hood will be at a minimum of 0.5 m/s. | |||
| E15 | Each fume hood will have a continuous monitoring device for proper functioning of the hood. An alarm, either visual or audible, will be present to indicate reduced air flow. | |||
| E16 | Prior to use, the fume hood will be tested to verify flow rate and the absence of counter-currents. | |||
| E17 | The fume hood will remain on at all times when nuclear substances are present.. | |||
| E18 | Provisions will be in place to ensure the fume hood remains functional if a routine automatic after-hours shutdown system is in place. | |||
| E19 | Fume hood exhaust fans will be connected to an emergency power system to maintain functionality if a power failure occurs. | |||
| E20 | Fume hoods will not contain filters. (If filtration will be required because nuclear substances will be released regularly through the fume hood exhaust or because biohazards are present, then detailed information about the filtration including filter monitoring and exchanges will be supplied.) | |||
| E21 | The fume hood exhaust will not connect to other exhaust systems. (If so, detailed information will be provided on the provisions made to ensure that the exhaust from one area cannot flow into another area.) | |||
| E22 | Fume hood exhaust ducts will be constructed of corrosion-resistant material appropriate to the substances to be used in the fume hood. All joints will be smoothly finished and sealed. | |||
| E23 | Fume hood exhaust ducts will be clearly identified on plans supplied to maintenance personnel. | |||
| E24 | Fume hood exhaust ducts will be marked at 3 meter intervals with the radiation warning symbol. | |||
| E25 | Fume hood exhaust ducts will contain only vertical sections. (If horizontal sections are to be used, detailed information will be submitted to show how collection of condensates or liquids coming in from the discharge point will be limited; horizontal ducts will slope at least 2.5 cm per 3 meters (1 inch per 10 feet) downward in the direction of the airflow to a suitable drain or sump.) | |||
| E26 | Fume hood exhaust fans will be placed close to the discharge point. | |||
| E27 | Fume hood exhaust fans will be located outside the building. | |||
| E28 | Fume hood exhausts will be located on the roof as far away as possible from any air intakes, to prevent recirculation of the fume hood emissions (the minimum recommended distance is 15.24m from an intake). | |||
| E29 | If the air intake will be less than 15.24m from the stack, rain caps on the stack will be avoided. | |||
| E30 | The stack velocity will be at least 1.4 times the average wind velocity. | |||
| E31 | The stack height will be at least 3.05m above the highest point on any adjacent roofline or air intake. Discharge will be directed vertically upward. | |||
| E32 | Stacks will be placed downwind of the air intakes (based on the average wind direction). | |||
| F | Shielding | Yes | No | Justification for variance included as separate attachment |
| F1 | Dose estimates to NEWs and non-NEWs in the area will be attached as part of this application (see Section 3.2 of this guide for details). | |||
| F2 | When appropriate, localized shielding will be used in areas where nuclear substances are to be used or stored depending on the quantities of nuclear substances that emit penetrating radiation. | |||
| F3 | When appropriate, shielding will be incorporated into the structure of the room. | |||
| F4 | A separate waiting room will be available for patients administered nuclear substances. | |||
| G | Miscellaneous | Yes | No | Justification for variance included as separate attachment |
| G1 | Food and drink preparation, use, and storage areas will not be present in the room unless required as part of a nuclear medicine procedure. Only patients undergoing studies may consume food or drink in the nuclear medicine rooms. | |||
| G2 | Office and study space will not be located near radioactive work areas. | |||
| G3 | Movement of nuclear substances will be minimized by locating in proximity those areas between which nuclear substances must be moved. | |||
| G4 | If the room or storage area is to be used for non-nuclear work as well, then separate labelled areas will be defined for the nuclear and non-nuclear work. | |||
| G5 | Rooms will have sufficient counter and floor space to allow people to work safely. (In general, allow at least 3 square meters of free floor space for each worker.) | |||
| G6 | An accessible area will be designated to store materials and equipment used for decontamination and monitoring (spill kits, survey meters where required, contamination meters where required). | |||
| G7 | Nuclear medicine departments will have washrooms dedicated for use by nuclear medicine patients. | |||
| G8 | Adequate space will be available for radioactive wastes generated by work within the nuclear substance laboratories or nuclear medicine rooms. This space may be within the lab/room or in a separate area. | |||
Glossary
- Air kerma
-
The kerma value for air, in gray, where kerma (K) is defined as:

where dEtr is the sum of the initial kinetic energies of all charged ionizing particles liberated by uncharged ionizing particles in air of mass dm. - ALARA
- “As Low As Reasonably Achievable”, social and economic factors being taken into account.
- Annual Limit on Intake (ALI)
- The activity, in Becquerels, of a radionuclide that will deliver an effective dose of 20 mSv during the 50-year period after the radionuclide is taken into the body of a person 18 years old or older or during the period beginning at intake and ending at age 70 after it is taken into the body of a person less than 18 years old.
- DAF
- Design Assessment Form; provided as Appendix C of this document.
- DCF
- Dose conversion factor; the committed effective dose in Sv, per unit activity in Bq, delivered by a given radionuclide of a given form. It is related to the ALI, in that the ALI can be calculated by dividing the DCF into 0.02 Sv (20 mSv).
- HTO
- Hydrogenated Tritium Oxide; also referred to as “tritiated water”.
- HVL
- See TVL/HVL.
- Nuclear Energy Worker (NEW)
- A person who is required, in the course of the person’s business or occupation in connection with a nuclear substance or nuclear facility, to perform duties in such circumstances that there is a reasonable probability that the person may receive a dose of radiation that is greater than the prescribed limit for the general public.
- Nuclear Medicine Room
- In the context of this guide, the term “nuclear medicine room” refers strictly to any area or enclosure that is used for the preparation of, or medical administration of, nuclear substances to persons via injection, inhalation, or ingestion, for the purpose of diagnosing or treating disease and for human research studies (excluding medical diagnostic x-rays or the medical use of sealed nuclear substances for brachytherapy or teletherapy treatments).
- Nuclear Substance Laboratory
- For the purposes of this document, any laboratory in which unsealed nuclear substances are used (also referred to as “radioisotope laboratory”).
- OBT
- Organically Bound Tritium.
- Occupancy Factor
- The fraction of total time during which a radiation field is present at a particular location, for which an individual is present at that location. For example, if a person spends four hours each day near a camera room that is fully occupied each hour of an eight-hour workday, then the occupancy factor is 0.5.
- PET
- Positron emission tomography; an imaging procedure that detects gamma rays that are emitted when positrons from a positron emitting source (such as F-18) collide with electrons in tissue.
- Poly-energetic source
- A source that has multiple radiation emissions of unique energies.
- TVL/HVL
- Tenth Value Layer; the thickness of material that attenuates 90% of the incident gamma rays (i.e., reduces the incident gamma rays to 10%). Similarly, the Half Value Layer is the thickness of material that attenuates 50% of the incident gamma rays (i.e., reduces the incident gamma rays to 50%).
References
The Web addresses (URLs) provided were functional at publication. Please note that Web addresses may change.
- Madsen, Mark, et al. AAPM Task Group 108: PET/CT Shielding Requirements. Medical Physics 33, 1 (January 2006): 4-15.
- International Commission on Radiological Protection. ICRP 68: Dose Coefficients for Intakes of Radionuclides by Workers.
- National Radiological Protection Board. NRPB-W22, Industrial Uranium Compounds: Exposure Limits, Assessment of Intake and Toxicity after Inhalation. 2002.
- National Council on Radiation Protection and Measurements (NCRP). NCRP Report No. 151: Structural Shielding Design and Evaluation for Megavoltage X- and Gamma-Ray Radiotherapy Facilities.
- NCRP. NCRP Report No. 124: Sources and Magnitude of Occupational and Public Exposures from Nuclear Medicine Procedures. NCRP, 1996.
- Hubbell, J.H. and Seltzer, S.M. Tables of X-Ray Mass Attenuation Coefficients and Mass Energy-Absorption Coefficients (version 1.4). National Institute of Standards and Technology, Gaithersburg, MD 2004.
- American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE). ASHRAE Handbook. ASHRAE, 2003.
- Stanford University. Stanford Laboratory Standard and Design Guide: Section 1 General Requirements for Stanford University Laboratories.
- Canadian Standards Association. CSA Z316.5-04—Fume Hoods and Associated Exhaust Systems. CSA, 2004.
- U.S. Department of Labor. Occupational Safety and Health Administration (OSHA) Technical Manual, Section III, Chapter 3
Additional Information
The following documents contain additional information that may be of interest to persons involved in designing, constructing, or renovating nuclear substance laboratories and nuclear medicine rooms.
The Web addresses (URLs) provided were functional at publication. Please note that Web addresses may change.
- American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE). Method of Testing Performance of Laboratory Fume Hoods. ANSI/ASHRAE 110-1995.
- ASTM International. C 1533-02 Standard Guide for General Design Considerations for Hot Cell Equipment. ASTM International, 2007.
- ASTM International. ASTM C 1554-03 Standard Guide for Materials Handling Equipment for Hot Cells.
- ASTM International. ASTM C 1572-04 Standard Guide for Dry Lead Glass and Oil-Filled Lead Glass Radiation Shielding Window Components for Remotely Operated Facilities.
- ASTM International. ASTM C 1615-05 Standard Guide for Mechanical Drive Systems for Remote Operation in Hot Cell Facilities.
- ASTM International. ASTM C 1217-00 Standard Guide for Design of Equipment for Processing Nuclear and Radioactive Materials. ASTM, 2006.
- Canadian Nuclear Safety Commission. R-52 rev. 1 Design Guide for Basic and Intermediate Level Radioisotope Laboratories. Ottawa, 1991. (Note: superseded by this document).
- Diberardinis, J., Baum, J., First, M., Gatwood, G., Seth A. Guidelines for Laboratory Design; Health and Safety Considerations. John Wiley and Sons Inc. 2001.
- European Committee for Standardization. BS EN 12469:2000 Biotechnology-Performance Criteria for Microbiological Safety Cabinets. 2000.
- Furr, A. Keith. CRC Handbook of Laboratory Safety, 5th Edition. CRC Press, 2000.
-
Health Canada,
Laboratory Biosafety Guidelines, 3rd edition, 2004.
- IAEA Safety Series 1, Safe Handling of Radioisotopes: Code of Practice (1973).
- International Organization for Standardization (ISO). ISO 10648-1:1997 Containment Enclosures– Part 1: Design Principles. ISO, 1997.
- ISO. ISO 10648 2:1994 Containment Enclosures– Part 2: Classification According to Leak Tightness and Associated Checking Methods. ISO, 1994.
- ISO. ISO 17873:2004 Nuclear Facilities—Criteria for the Design and Operation of Ventilation Systems for Nuclear Installations Other than Nuclear Reactors. ISO, 2004.
- ISO. ISO 17874-1:2004 Remote Handling Devices for Radioactive Materials—Part 1: General Requirements. ISO, 2004.
- ISO. ISO 17874-2:2004 Remote Handling Devices for Radioactive Materials—Part 2: Mechanical Master-Slave Manipulators. ISO, 2004.
- ISO. ISO 17874-4:2006 Remote Handling Devices for Radioactive Materials—Part 4: Power Manipulators. ISO, 2006.
- ISO. ISO 17874-5:2004 Remote Handling Devices for Radioactive Materials—Part 5: Remote Handling Tongs. ISO, 2004.
- National Institute of Health. NIH Guidelines for Research Involving Recombinant DNA Molecules. U.S. Department of Health, Education and Welfare, April 2002.
- Occupational Health and Safety Administration. National Research Council Recommendations Concerning Chemical Hygiene in Laboratories (Non-Mandatory). 1910.1450 Appendix A.
- Princeton University. Laboratory Safety Manual.
- RWDI Consulting Engineers and Scientists. TECHNOTES, Issue No 16, Air Intake Placement for Laboratories—A General Overview.
- U.S. Department of Health and Human Services, Biosafety in Microbiological and Biomedical Laboratories, Fifth Edition, 2007.
- U.S National Science Foundation. NSF/ANSI 49-2004A Class II (laminar flow) Biohazard Cabinetry. NSF 2004.
- World Health Organization. Laboratory Biosafety Manual 3rd edition. WHO, 2004.
Page details
- Date modified: